Sources:
1. Fargen, Kyle, Arthur, Adam, Mazwi, Thabele et al., A survey of burnout and professional satisfaction among United States neurointerventionalists J Neurointerv Surg, November 2019, Vol. 11:11, pp. 1100-1104
2. Wilson TA, Leslie-Mazwi T, Hirsch JA, et al. A multicenter study evaluating the frequency and time requirement of mechanical thrombectomy. J Neurointerv Surg 2018;10:235–9.
3. Jha, Ashish, Iliff, Andrew, Chaoui, Alain, et al. A Crisis in Health Care: A Call to Action on Physician Burnout, Partnership with the Massachusetts Medical Society, Massachusetts Health and Hospital Association, Harvard T.H. Chan School of Public Health, and Harvard Global Health Institute, 2019
4. Han, Shasha, Shanafelt, Tait , Sinsky, Christine, et al. Estimating the Attributable Cost of Physician Burnout in the United States, Annals of Internal Medicine, June 4, 2019, doi.org/10.7326/M18-1422
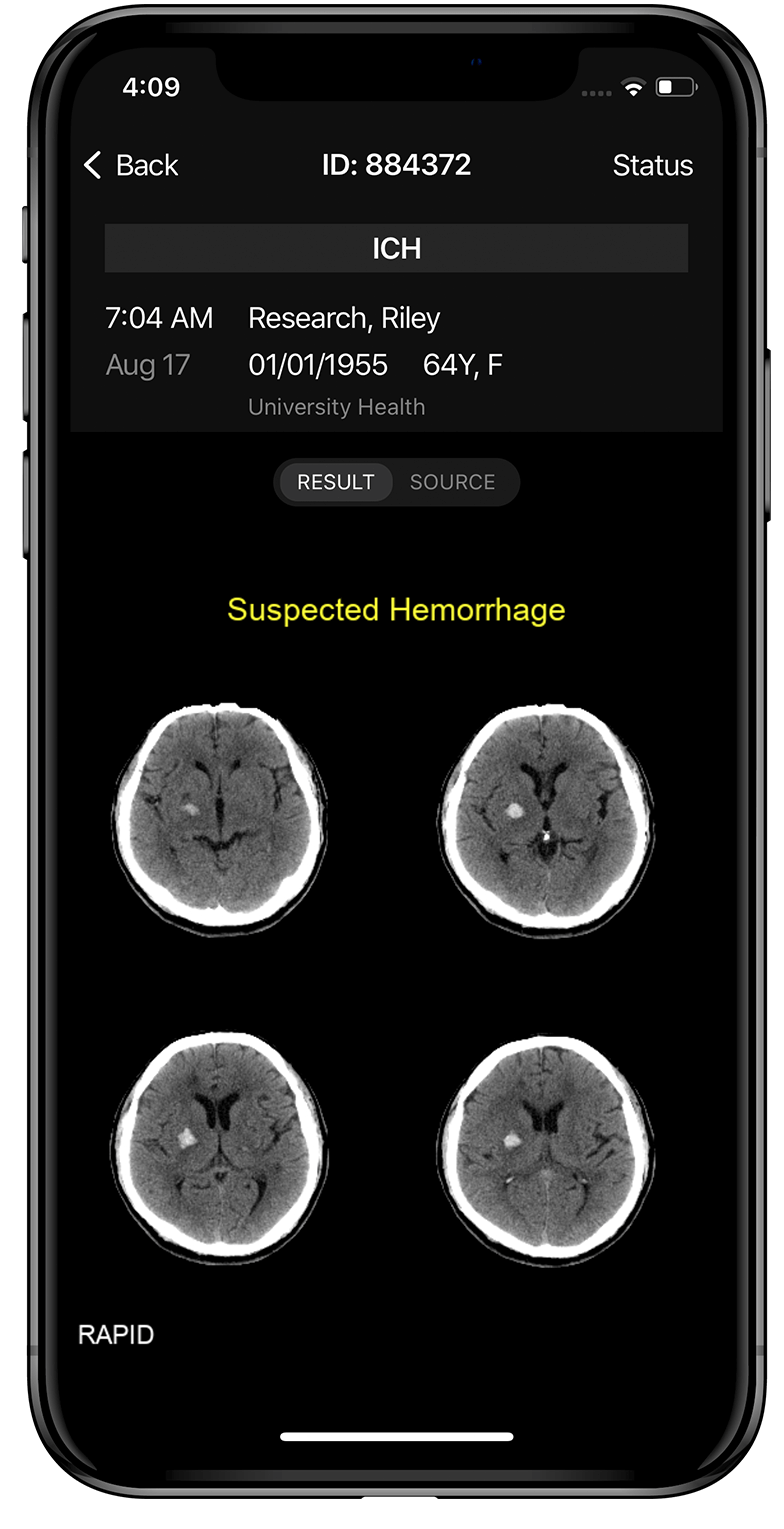
5. Seena Dehkharghani, Seena, Lansberg, Maarten, Venkatsubramanian, Chitra et al., High-Performance Automated Anterior Circulation CT Angiographic Clot Detection in Acute Stroke, Radiology 2021; 00:1–6