Take a look back at how stroke diagnosis and treatment has changed over time.
“It is impossible to cure a severe attack of apoplexy and difficult to cure a mild one.” – Hippocrates
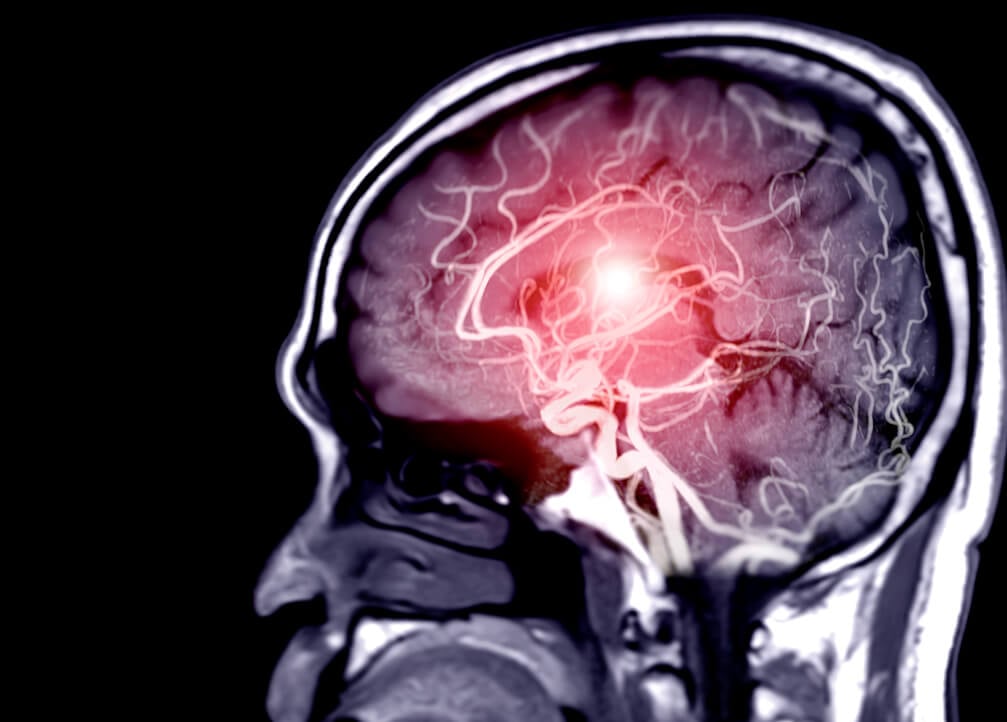
Although these words were written about stroke some 2,400 years ago, referring to the condition by its earlier name apoplexy, they held true all the way up to the late 20th century when the first medical treatment for stroke finally emerged. Since then, new drugs and procedures have become available, while advanced imaging tools have given physicians unprecedented views of the brain to help with stroke diagnosis and treatment decisions.
Take a look back at how stroke diagnosis and treatment has changed over time.
Johann Jacob Wepfer, a physician practicing in Switzerland, identified the root causes of stroke. Based on postmortem examinations of people who had died of the condition, Wepfer identified two forms of stroke that modern medicine still distinguishes between today: ischemic and hemorrhagic.
Dr. Amos Twitchell performed the first documented carotid artery surgery in the United States. By operating on the carotid arteries to reduce cholesterol buildup, surgeons could remove blockages that could potentially lead to a stroke, but a method for treating an existing stroke would not be available to physicians until the following century.
Physicist Wilhelm Conrad Röntgen became the first person to observe X-rays, a significant advancement that allowed for unprecedented insights into the bodies of living patients; the skull and protective cerebrospinal fluid, however, greatly limited the quality of early diagnostic images of the brain.
The development of computed tomography (CT) led to a breakthrough in stroke diagnostics. For the first time, physicians could reliably discern whether they were dealing with a circulatory problem or a cerebral hemorrhage. The emergence of magnetic resonance imaging (MRI), meanwhile, allowed further information to be obtained about a stroke.
Tissue plasminogen activator (tPA), a drug that breaks down a clot by dismantling its underlying framework, became the first FDA-approved medical treatment for ischemic stroke. It was originally approved to treat acute ischemic stroke within 3 hours of symptom onset.
The American Heart Association endorsed mechanical thrombectomy as a standard method for treating ischemic stroke up to 6 hours after symptom onset. In this procedure, physicians pass a catheter into the groin and through the carotid artery to remove a blood clot.
The Rapid imaging system was used for patient selection in two landmark clinical trials, DAWN and DEFUSE 3, which proved that stroke patients could successfully be treated with thrombectomy up to 24 hours after symptom onset. The results of these studies led the American Heart Association to expand its recommended stroke treatment window from 6 to 24 hours, greatly increasing the number of patients eligible for life-saving treatment.
Using Rapid imaging to determine patient eligibility, the EXTEND trial proved that intravenous tPA can be effective for acute ischemic stroke up to 9 hours after symptom onset or double the original treatment window.
The Rapid platform received FDA clearance to identify suspected large vessel occlusions in ischemic stroke patients (Rapid LVO) and to notify physicians of possible intracranial hemorrhage (Rapid ICH), becoming a truly comprehensive solution for both ischemic and hemorrhagic stroke. It also became the first-ever neuroimaging solution to receive FDA clearance in the CADx (Computer-Assisted Diagnostic software) category for its Rapid ASPECTS product.
The Rapid platform has been validated in a dozen more major clinical trials and is now used in more than 1,800 hospitals worldwide.

Machine learning and other stroke artificial intelligence (AI) techniques are changing medicine in profound ways. At RapidAI, we are using it to extract greater meaning from medical imaging data and to develop tools that ultimately help physicians improve patient care.